Abstract

Background: Survival among patients diagnosed with acute promyelocytic leukemia (APL) has significantly improved with the use of all-trans retinoic acid (ATRA) and arsenic trioxide (ATO). However, the need for immediate diagnosis, access to specialized care and complexity and cost associated with APL management can potentially act as a barrier for disadvantaged patients. Whether socio-economic factors influence the outcomes of patients with APL remains unclear.
Methods: We used data from the National Cancer Institute's Surveillance Epidemiology and End Results program (SEER-18) to analyze APL cases diagnosed in patients < 65 years of age between 2007 (year when insurance information became available) and 2015 (most recent year available) to characterize the impact of insurance, marital status, county-level income, county-level educational achievement and residence in rural or urban county on survival. Cases were grouped according to age (< 40 years and ≥ 40 years), and analyzed considering race/ethnicity, gender, and year of diagnosis.
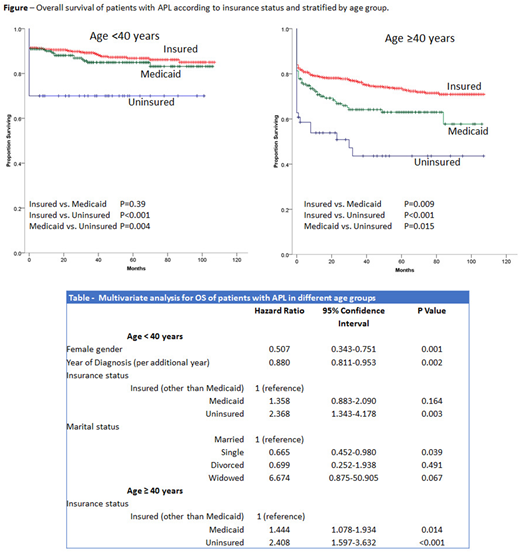
Results: A total of 1,787 APL cases (816 < 40 years and 971 ≥ 40 years) were included in the analysis with a median follow up of 35 months (0-107). The median age at diagnosis was 41 years (0-64 years), 52.5% were male, 52.3% non-Hispanic Whites (NHW), 11.8% non-Hispanic Blacks (NHB), 25.9% Hispanics and 9.9% of other race/ethnicity. Marital status was single for 36.9%, married for 54%, divorced for 7.5% and widowed for 1.6%. Among patients <40 years, 64% were insured (other than Medicaid), 29.9% were Medicaid beneficiaries and 6.1% uninsured. Among patients ≥ 40 years figures were 77.1%, 17.6% and 5.3% respectively. For age < 40 years, patients with insurance (other than Medicaid) and Medicaid had improved survival compared to patients without insurance. There was no statistically significant difference between Medicaid and other insurance (Figure). Among patients ≥ 40 years, being insured (other than Medicaid) was associated with higher survival than being Medicaid beneficiary or being uninsured, while patients with Medicaid had better survivals than uninsured patients (Figure). In multivariate analysis of patients < 40, higher risk of death was associated with being male, diagnosis in earlier years and being uninsured while lower risk of death was associated with being single (Table). Other socioeconomic variables did not contribute to the model. For patients ≥ 40 years, mortality was increased for both Medicaid and uninsured patients compared to insured patients (Table). No other demographic or socioeconomic variable contributed to the model.
Conclusion: Despite the high cure rate experienced by patients with APL, patients < 65 years without insurance and those ≥ 40 with Medicaid are at significant disadvantage compared to patients with insurance. These findings point to an opportunity to improve survival in APL by addressing access to care.
Costa:Abbvie: Research Funding; Amgen: Honoraria, Research Funding; Karyopharm: Research Funding; BMS: Research Funding; Celgene: Honoraria, Research Funding; Janssen: Research Funding; Sanofi: Honoraria.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal